This website uses cookies so that we can provide you with the best user experience possible. Cookie information is stored in your browser and performs functions such as recognising you when you return to our website and helping our team to understand which sections of the website you find most interesting and useful.
Patient Name: Mrs X
Nurse Name: Jenny Marsden and Fiona Brown
Patient Care Setting: York Teaching Hospital NHS Foundation Trust
Patient Overview: A 48 year old female was admitted electively for paraumbilical hernia repair. Normally fully mobile and active, working, enjoys swimming and lives with her partner. Known to have alcoholic liver disease with associated ascites, and being treated medically with TDS lactulose.
Admitted acutely 3 days later with ischaemic bowel, and underwent emergency right hemicolectomy with formation of double barrelled ileostomy. Difficult procedure due to the ascites, bowel brought out under some tension to within the lower end of previous minilaparotomy suture line, and flush to skin.
Extended hospital stay- 4weeks, due to high stoma output, and associated management of fluid balance and pouch change/reliability.
Acceptable fluid balance and stable bloods achieved with loperamide and codeine doses, output loose, 800-900mls in 24 hours.
Discharged home over the Christmas period, patient was independent, and had achieved reliability with Dansac Tre seal and Coloplast sensura mio flat high output pouch.
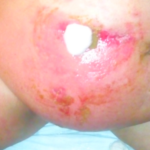
Problem: Developed increased problems over the New Year holiday 3/1/19 and eventually sought review 7/1/19 when she could not get a pouch to adhere over the weekend.
Suspected Cause: High, loose output, flush stoma sitting within her minilaparotomy suture line, distended abdomen. Patient compliance and knowledge- she had left pouch off on the Sunday, leaving skin fully exposed, cleansing skin when necessary, not aware she could and should have sought review over the weekend as a ward attender.
Peristomal moisture related skin damage with associated increasing trans epidermal water loss.
Course of treatment: Admitted 7/1/19 (see photo) for skincare management. Continued with previous products, ilex paste applied to immediate area surrounding stoma bud. Photographic care plan provided for ward staff to assist patient during pouch change.
Some improvement in pouch wear time, but still only lasting 3-4 hours before needing change.
9/1/19 slight improvement in condition of skin and pouch wear time.
Changed product use to Tre seal and Pelican Platinum with Vit E convex high output pouch.
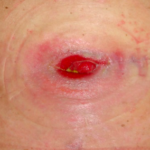
10/1/19 Skin improving and pouch reliability much improved to 10hours.
14/1/19 Skin improving, with minimal trans epidermal water loss form the extended/wider area, and pouch reliability improved to 48 hours.
16/1/19 Skin much improved, pouch reliability continues 48hours. Discharged home.
- 3/01/19
- 07/01/19 Admitted
- 09/01/19
- 10/01/19
- 14/01/19
- 16/01/19 Discharged
Interventions/complications? Patient developed suspected pyoderma gangrenosum ulcers (not biopsied). Probable suture sites from minilaparotomy, but were also in position with the pouch belt loops. Treated with Tacrolimus topical steroid for 2-3 weeks with good results, belt loops cut off pouch initially, but then left insitu with gauze for padding when using belt.
Outcome: Patient’s skin rapidly improved. Consequent improved comfort with better pouch adherence and reliability. This has ensured increased patient confidence. She is sleeping better and feels confident to resume normally daily activities for her including swimming.
Conclusions: Change of products has improved patient’s confidence and quality of life, reduced patient stay and expedited discharge from hospital, extended wear time and less accessories used saving the NHS money.
Don't forget to share this post!